skin cancer
Skin Cancer Explained
Skin cancer is the most common cancer in Australia, and it’s something that affects thousands of people every year—including those who are vigilant about sun protection and regular skin checks.
If you’ve recently been diagnosed with a suspicious mole or skin lesion, or have a history of skin cancer, you might feel overwhelmed by the medical jargon, the steps involved in treatment, and what to expect next.
This page is here to help you understand the process, from early detection to ongoing care, so you can feel empowered and informed about your health.
What is skin cancer?
Skin cancer occurs when skin cells grow abnormally, usually due to damage from ultraviolet (UV) radiation from the sun or tanning beds. There are three main types of skin cancer:
-
Basal Cell Carcinoma (BCC)
The most common and least dangerous form. It grows slowly and rarely spreads. -
Squamous Cell Carcinoma (SCC)
Can grow more quickly and may spread if not treated. -
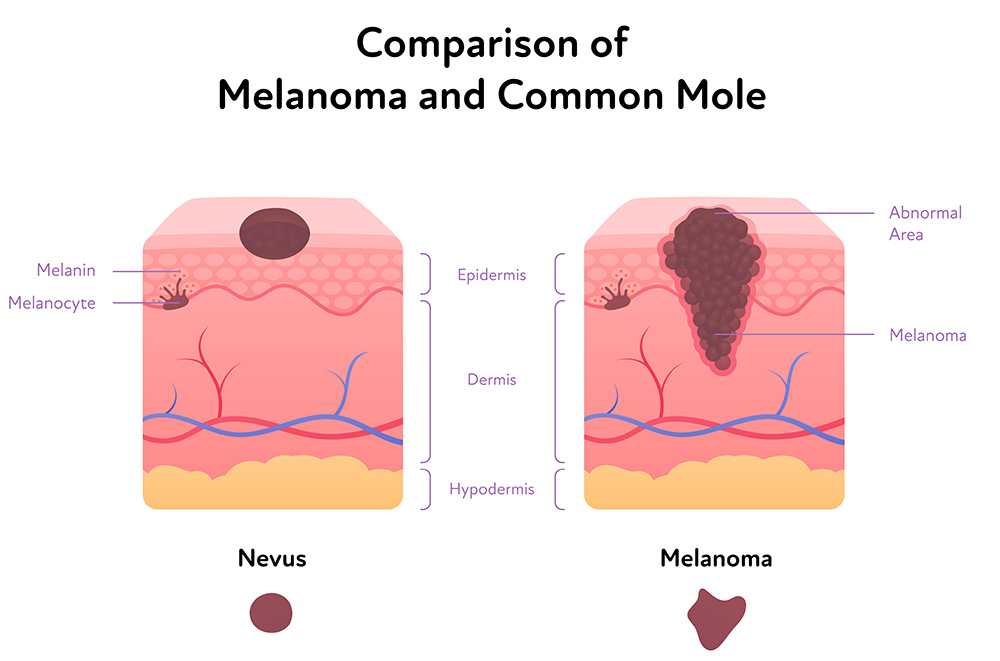
Melanoma
The most serious type. It can spread to other parts of the body and become life-threatening if not detected early.
Early detection matters!
Early detection is crucial. When found early, most skin cancers can be treated successfully. Regular skin checks—either self-examinations or by a doctor—can help catch changes before they become serious.
What to Look Out For
Knowing what to look for on your skin can save your life. Here’s what you should keep an eye on:
- A – Asymmetry
One half of the mole doesn’t match the other. - B – Border
Edges are irregular, ragged, or blurred. - C – Colour
Uneven colour, with shades of brown, black, tan, red, white, or blue. - D – Diameter
Larger than 6mm (about the size of a pencil eraser), though melanomas can be smaller. - E – Evolving
Any change in size, shape, colour, or elevation—or new symptoms such as bleeding, itching, or crusting.
Other warning signs
A sore that doesn’t heal
A new growth or spot could be a skin cancer risk
A spot that looks different from others (“ugly duckling” sign)
Redness or swelling beyond the border of a mole
Sensation changes, such as itchiness, tenderness, or pain
If you notice any of these signs, please talk to one of our GPs below.
GPs with a special interest in skin cancer
All skin doctors at The Woods Medical Centre have completed extensive training in the detection, management and treatment of skin cancer.
approach to skin cancer
The Diagnosis Process
A doctor will examine your skin, often using a dermatoscope (a magnifying tool). They may photograph lesions to track changes over time.
2. Biopsy
If a suspicious spot is found, your doctor will usually perform a biopsy. This involves removing all or part of the lesion so it can be examined under a microscope.
Shave Biopsy: Removes the top layers of skin.
Punch Biopsy: Removes a small, deeper sample.
Excisional Biopsy: Removes the entire lesion with a margin of normal skin.
3. Pathology Results
A pathologist examines the tissue to determine if cancer is present, and if so, what type and how advanced it is.
- Further reading: Types of Skin Cancer WA (Skin Cancer WA)
What are margins?
- Margins refer to the border of healthy tissue around the removed lesion.
- For melanoma, guidelines usually recommend removing an additional margin of normal skin—often 5mm or more, depending on the depth and type of cancer.
- This reduces the risk of cancer cells being left behind, which could lead to recurrence.
Why Is Further Surgery Needed?
- The initial biopsy may not remove all the cancerous cells.
- Pathology may show that the margins are “involved” (cancer cells are present at the edge), so a wider excision is needed.
- Further surgery ensures the best chance of a cure and lowers the risk of the cancer returning or spreading.
- To ensure that cancer is removed according to evidence-based research into margins and recurrence.
Staging and Further Tests
If melanoma or another aggressive skin cancer is found, your doctor may refer you to a specialist for further testing to check if the cancer has spread (metastasised):
-
Lymph Node Examination
Feeling for enlarged nodes or using ultrasound. -
Sentinel Lymph Node Biopsy
A special procedure to check the first lymph node cancer is likely to spread to. -
Imaging
PET scans, CT scans, or MRIs may be used in advanced cases.
Types of skin cancer
Basal cell carcinoma
The most common type, accounting for about 2 out of 3 skin cancers. BCCs rarely spread but can cause significant local damage if left untreated.
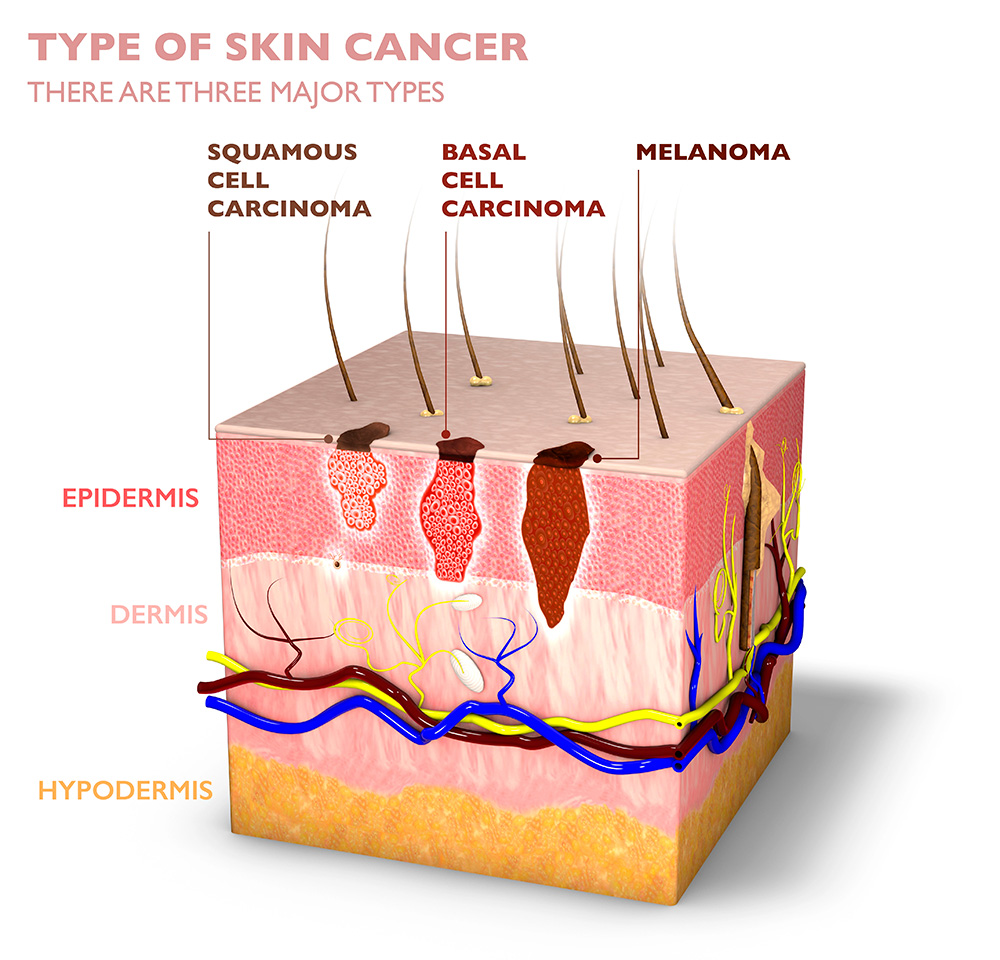
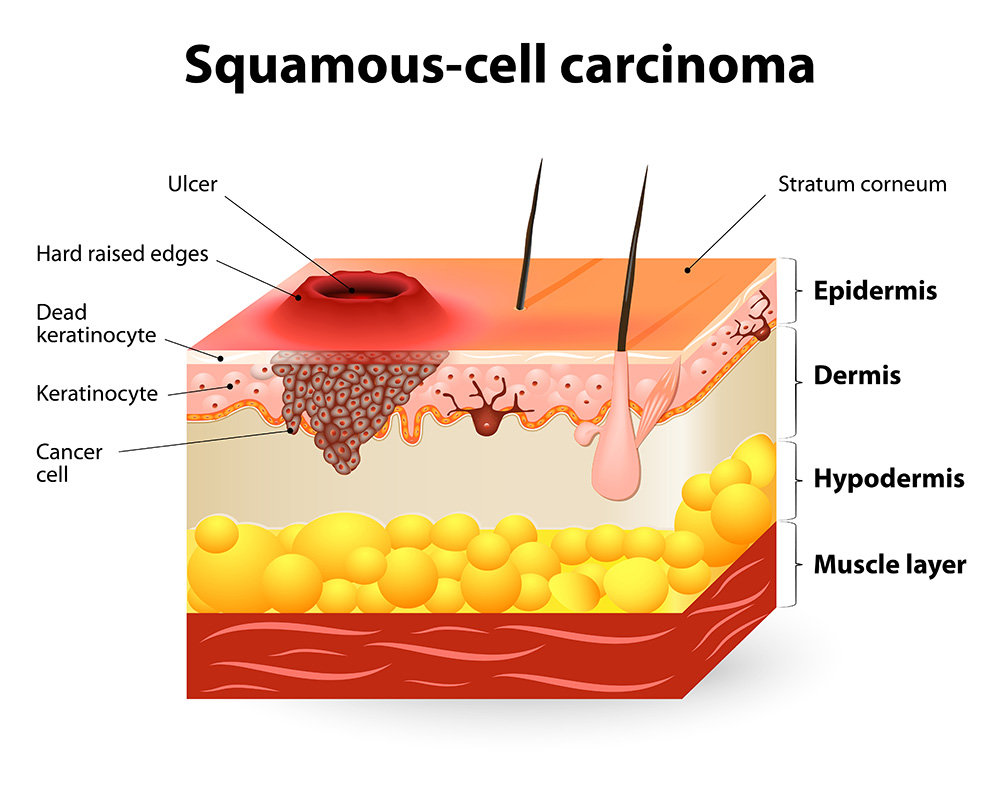
Squamous cell carcinoma
The second most common type, making up about 1 in 3 skin cancers. SCCs have a higher risk of spreading than BCCs if not treated promptly.
Melanoma
While less common (about 1 in 100 skin cancers), melanoma is the most serious form due to its higher likelihood of spreading to other parts of the body if not detected early. It is the third most commonly diagnosed cancer in Australia (excluding non-melanoma skin cancers).
Treatment Options
Surgical treatments
- Excision (simple, flap or graft)
The most common treatment. The cancer and a margin of healthy tissue are removed. - Mohs Surgery (specialist referral required)
A specialised technique, often for facial cancers, where tissue is removed layer by layer and examined until no cancer remains.

Non-surgical treatments
- Topical Treatments
Creams or gels for certain early skin cancers. - Cryotherapy
Freezing the cancer cells (used for some superficial skin cancers). - Radiation Therapy
Used in some cases where surgery isn’t possible. - Immunotherapy/Targeted Therapy
For advanced or metastatic melanoma.
What to expect after treatment
Recovery
Most excisions heal within a few weeks.
You may have stitches and a scar, which usually fades over time.
Your doctor will provide wound care instructions.
Follow up
Regular follow-up visits are essential—especially if you’ve had melanoma or multiple skin cancers.
Your doctor will check for recurrence and new skin cancers.
You may need more frequent skin checks (every 3–6 months) for several years.
Emotional impact
A skin cancer diagnosis can be frightening and stressful.
It’s normal to feel anxious about recurrence or new lesions.
Support is available—talk to your doctor, a counsellor, or join a support group if you need help coping.
Preventing skin cancer
- Use Sunscreen
SPF 30+ every day, even on cloudy days. - Wear Protective Clothing
Hats, sunglasses, and long sleeves. - Seek Shade
Especially during peak UV hours (10am–4pm). - Avoid Tanning Beds
They increase your risk of melanoma. - Regular Skin Checks
Self-examine monthly and see your doctor for annual checks or more often if you’re high-risk.

Your story matters
Many people are surprised by how much is involved after a skin cancer diagnosis. It’s not just about removing a mole—sometimes, it means more surgery, ongoing checks, and learning to live with uncertainty. But with early detection and proper care, most people recover fully and live healthy lives.
If you have questions or concerns about your skin, don’t wait—book a skin check today. Your health is worth it.
Actinic Keratosis
(solar keratosis)
These are common rough, scaly patches on the skin caused by sun exposure and are considered pre-cancerous lesions. Up to 10% of AKs can develop into SCCs if left untreated.
Australia has one of the highest incidences of AKs in the world, with an estimated prevalence of 37-55% in Australian adults over 40.
Resources & Support
How often do I need a skin check?
Regular skin checks are recommended for everyone
If you notice a new spot, or any mole that is changing in size, shape, colour, or is bleeding, itching, or painful, please book an appointment immediately.
Get checked if you . . .
- Have a personal history of skin cancer.
- Have a family history of melanoma.
- Have many moles, or moles that are large, unusual, or changing.
- Have fair skin, a history of significant sun exposure, or multiple past sunburns.
- Are over the age of 40 (even if you have none of the above risk factors).
