onychocryptosis
Ingrown toenail
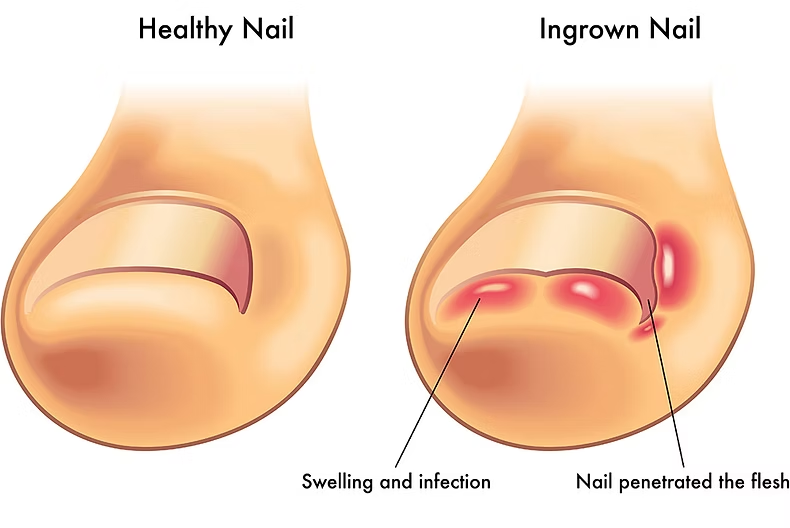
An ingrown toenail can be a painful condition that can become infected and may require surgical treatment.
The epidemiology of onychocryptosis is difficult to determine as it is often considered to be a minor medical problem and as such has been some-what neglected in the literature.
What is an ingrown toenail?
What causes an ingrown toenail?
Several factors can contribute to an ingrown toenail developing:
- Improperly trimmed nails
Cutting your toenails too short, especially rounding the corners instead of trimming straight across, can encourage the nail to grow into the skin. - Tight-fitting footwear
Shoes that are too narrow, too short, or put pressure on your toes can jam your nails into the surrounding flesh. - Toe injuries
Stubbing your toe, dropping something on it, or other trauma can sometimes lead to an ingrown nail. - Nail shape: Some people are just more prone to ingrown toenails due to naturally curved or “pincer” nails.
- Poor foot hygiene
While not a direct cause, neglecting foot care can increase the risk of complications if an ingrown nail develops. - Repetitive activities
Activities that put repeated pressure on your toes, like kicking a soccer ball, can contribute.

How do you know you have an ingrown toenail?
Common symptoms include:
- Pain and tenderness: The affected area will be sore to the touch.
- Redness and swelling: The skin around the nail will appear inflamed.
- Pus or drainage: In more severe cases, especially if infected, you might see pus or clear fluid.
- Warmth: The area might feel warm to the touch.
- Overgrowth of skin: Sometimes, the skin around the nail can start to grow over the nail itself.
When to see your GP
While some mild cases of ingrown toenails can be managed at home, it’s important to know when to see your GP. You should seek help if:
- You have diabetes, poor circulation, or any other condition that affects blood flow to your feet. These conditions can make you more susceptible to serious infections.
- The pain is severe or getting worse.
- There are signs of infection (pus, increasing redness, warmth, fever).
- You’ve tried home remedies for a few days and there’s no improvement.
- The problem is recurring frequently.
Homecare tips
For mild cases only
-
Soak your foot
Soak the affected foot in warm water with Epsom salts for 15-20 minutes, 3-4 times a day. This can help reduce swelling and tenderness. -
Gently lift the nail
After soaking, you can try to gently lift the edge of the ingrown nail and place a small piece of clean cotton or dental floss underneath it. This helps guide the nail to grow over the skin. Change the cotton or floss daily. -
Over the counter pain relievers
Paracetamol or ibuprofen can be taken to help manage pain and inflammation.
Important
Do not try to dig out the ingrown nail yourself, as this can worsen the condition and lead to infection.
Preventing ingrown toenails in the first place...
The good news is that many ingrown toenails can be prevented with a few simple practices:
- Trim your toenails correctly:
- Always cut them straight across, not in a curve.
- Avoid cutting them too short; leave a little white tip.
- Don’t tear or pick at your toenails.
- Wear properly fitting shoes:
- Choose shoes with a wide toe box that allows your toes to wiggle freely.
- Avoid high heels and pointy-toed shoes that can compress your toes.
- Keep your feet clean and dry: Good foot hygiene can help prevent infections.
- Inspect your feet regularly: Pay attention to any changes in your toenails or skin.
Partial Toenail Wedge Resection
Surgical removal of a wedge of toenail tissue for ingrown toenails
A partial toenail wedge resection is a surgical procedure to remove a wedge of nail tissue from the side of a toenail. It is most commonly performed to treat ingrown toenails, which occur when the nail grows into the skin at the side of the toe. Ingrown toenails can be painful, red, and swollen, and they may become infected.
When is a Partial Toenail Wedge Resection necessary?
A partial toe wedge resection may be necessary if you have an ingrown toenail that is not responding to conservative treatment, such as above.
If you have an ingrown toenail that is causing pain, swelling, or infection, Dr. Atish Chudasama may be able to help. Dr Chudasama may prescribe antibiotics, or recommend a partial toe wedge with phenolisation (a surgical procedure used to treat ingrown toenails).
This procedure is common and effective. Think of it as a two-part solution

TL;DR
Risks and benefits of partial toe wedge resection
- Pain relief
- Prevention of further ingrown toenails
Chances of success?
Partial toenail wedge resection with phenolisation has a very high success rate, typically ranging from 90% to 98% in permanently resolving the ingrown toenail issue. This makes it one of the most effective treatments for recurrent ingrown toenails.
What are the risks of complications?
While generally safe and routinely performed, like any procedure, there are potential risks, though serious complications are rare:
- Infection: Despite sterile techniques, there’s a small risk of infection at the surgical site. This can usually be managed with antibiotics.
- Pain and Discomfort: You’ll experience some discomfort as the local anaesthetic wears off, but this is usually manageable with over-the-counter pain relief.
- Prolonged Weeping/Discharge: The phenol can cause the treated area to weep or discharge for a few days to a few weeks as it heals. This is a normal part of the healing process as the dead tissue separates.
- Re-growth: In a small percentage of cases (2-10%), the portion of the nail that was treated may partially or fully grow back. If this happens, the procedure can often be repeated.
- Adverse Reaction to Phenol: While rare, some individuals may have a localised reaction to the phenol, leading to more prolonged inflammation.
- Scarring: There’s usually minimal scarring, as the procedure doesn’t involve cutting the surrounding skin in the same way a traditional wedge resection might.
- Allergic Reaction: As with any medication, there’s a rare risk of allergic reaction to the local anaesthetic or other materials used.
- Granuloma Formation: Occasionally, a small lump of tissue (granuloma) can form at the site, which usually resolves with simple treatment.
What is the recovery time?
Recovery from a partial toenail wedge resection with phenolisation is generally quick:
Immediately After
Your toe will be numb for a few hours due to the local anaesthetic. A dressing will be applied.
First 24-48 Hours
Rest and elevation of your foot are recommended to reduce swelling and discomfort. You can usually walk immediately after the procedure, but avoid strenuous activity.
First Few Days to 1 Week
You can typically resume most light daily activities and wear open-toed shoes or sandals. You’ll need to follow specific dressing change instructions as instructed by your GP. Some mild pain, throbbing, or weeping from the site is normal.
Full Healing
While you can usually get back to most activities quite quickly, the surgical site can take 2 to 6 weeks (or sometimes longer) to fully dry and heal. The length of healing can depend on individual factors and if there was a pre-existing infection.
Strenuous Activity/Sports
Avoid high-impact exercise or strenuous activities for approximately 2 to 4 weeks, or as advised by your doctor.
What should I do to care for my toe after the procedure?
Proper aftercare is vital for optimal healing and to minimise complications
Keep Dressings On
Follow your doctor’s instructions regarding how long to keep the initial dressing on (often 24-48 hours). Keep it clean and dry.
Dressing Changes
You’ll be given specific instructions on how to change your dressings at home.
Pain Management
Take over-the-counter pain relief (like paracetamol) as directed if you experience discomfort. Avoid aspirin or ibuprofen unless specifically advised, as they can sometimes increase bleeding risk.
Elevation
Keep your foot elevated as much as possible for the first 24-48 hours to help reduce swelling and throbbing.
Footwear
Wear open-toed shoes, sandals, or thongs for at least the first week to avoid pressure on the treated toe.
Hygiene
You can usually shower after 24-48 hours (or as advised), but ensure the toe is gently cleaned and thoroughly dried afterwards. Avoid prolonged soaking (e.g., baths or swimming) until the wound has fully closed and healed.
Activity
Gradually return to normal activities. Avoid heavy lifting or strenuous exercise initially.
Monitor for Complications
Watch for signs of infection such as increasing pain that doesn’t respond to medication, excessive redness spreading from the site, worsening swelling, pus, fever, or chills. Contact us if you notice any of these.
Follow-Up Appointments
Attend all scheduled follow-up appointments with your doctor. These are crucial for monitoring healing and addressing any concerns.
Useful Links
An ingrown toenail can be a painful condition that can become infected and may require surgical treatment. The epidemiology of onychocryptosis is difficult to determine as it is often considered to be a minor medical problem and as such has been some-what neglected in the literature.
- Ingrown toenails and the role of your GP (RACGP website)
Ingrown toenails become more common in older people as the nails get thicker with age. They are more likely to become infected in people who have diabetes or circulation problems.
- More about ingrown toenails (HealthDirect)
